The cornea and sclera form the tough outer layer of the eye-wall. These tissues serve a multitude of functions. The transparent cornea provides two thirds of the refractive power of the eye. The sclera serves to mechanically support the retina and to maintain an optimal shape for vision in the presence of physiological fluctuations in the intraocular pressure. Myopia and hyperopia, also known as nearsightedness and farsightedness, are caused by the axial lengthening and shortening of the sclera, which misaligns the retina with the focal plane. The cornea and sclera together also serve to protect the delicate internal components of the eye, such as the lens, from external injuries. The mechanical properties of the cornea and sclera arise from the anisotropic fibrous microstructure of the stroma, which contains densely stacked lamellae primarily of type I collagen fibrils embedded in a hydrated matrix of proteoglycans.
Our lab seeks develop advanced experimental methods and micro-mechanical models to investigate the relationship between the collagen structure, mechanical properties, and physiologicall function of the cornea and sclera, and their alterations with age and disease.
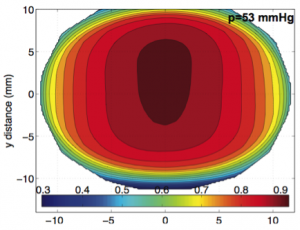
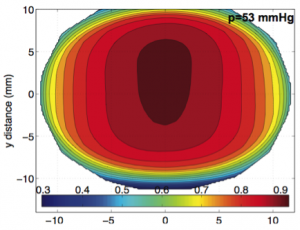
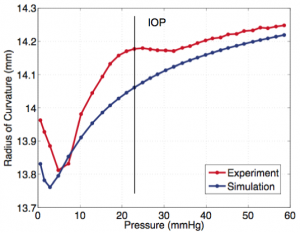
Figure 1. Finite element simulation of the inflation response of bovine cornea, showing (a) a specimen specific model of an inflation test specimen, where the arrows indicate the orientation of collagen fibers; (b) the out-of-plane displacement caused by inflation from 1 mmHg to 45 mmHg; (c) a plot of the curvature of the cornea vs. pressure comparing simulations and inflation test measurements using 3D digital image correlation (DIC).
Scleral biomechanics in glaucoma
The sclera is a dynamic biological tissue that undergoes physiological changes with age and pathological changes with diseases, such as glaucoma. Studies have shown that the human and monkey sclera stiffen and creep more slowly with age. Glaucoma is a blinding disease characterized by progressive degeneration of the axons of retinal ganglion cells. The degree of fiber alignment is significantly lower in the superior-temporal and inferior-nasal quadrants in the peripapillary region, immediately adjacent to the optic nerve head, of glaucoma eyes. Uniaxial strip tests and inflation tests of the sclera consistently measure a stiffer mechanical response and altered viscoelastic properties for glaucoma eyes in humans and animal models of the disease. Dramatic alterations in the mechanical behavior and structure have also been measured in myopia, where the sclera thins and elongates in response to the quality of the image focus on the retina. The sclera of induced-myopia chick and tree shrew eyes are significantly more compliant and exhibit faster creep than the sclera of contralateral control eyes.
Our research aims to:
- Measure the mechanical properties and collagen structure of the posterior sclera using inflation test with digital image correlation (DIC) and wide angle x-ray scattering (WAXS).
- Compare for the effects of age and glaucoma.
- Determine how the extracellular matrix structure influence the mechanical properties.
- Develop microstruture-based constitutive model for the sclera that incorporates explicitly the WAXS measurements of collagen structure.
- Computationally model the effect age and disease induced variation in scleral properties and structure on the deformation of the tissues of the optic nerve head.
- Develop micromechanism-based constitutive models for the growth and remodeling of the tissues in response to mechanical loading
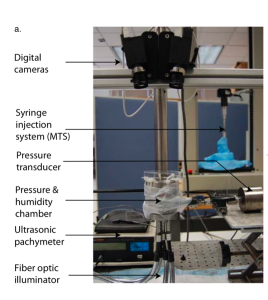

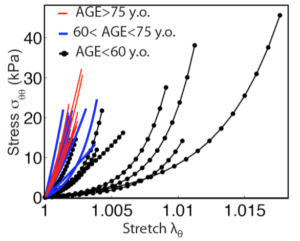
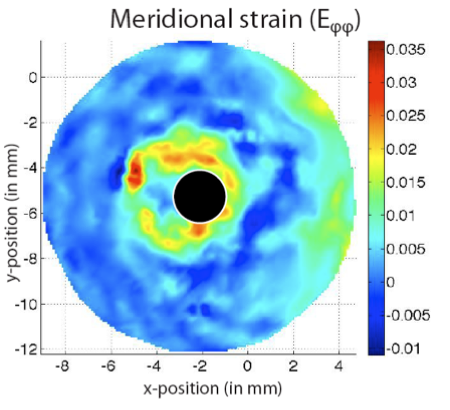
Figure 2. Inflation test with 3D DIC of the human posterior sclera, showing (a) the inflation test setup; (b) the contour of the meridional strains measured by 3D DIC that shows a large strain concentration around the optic nerve head and (c) the average meridional stress vs. stretch for the inflation tested specimens in different age groups.
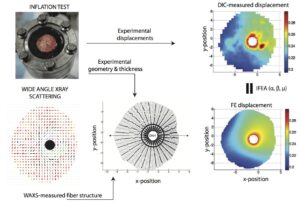
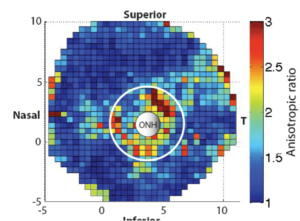
Figure 3. Micromechanical model of the human posterior sclera, showing (a) a schematic of the inverse finite element method that used specimen-specific models to fit the material parameters of anisotropic hyperelastic constitutive model to the full field displacement response to inflation measured by 3D DIC; and (3) the simulation of the circumferential stress in the posterior sclera caused by inflation from 1 mmHg to 45 mmHg.
Mouse model of glaucoma
Experiments have shown that the sclera of human glaucoma eyes show exhibit large variation in the mechanical properties and collagen structure from that of age-match glaucoma eyes. Whether these differences are natural variations that predisposes an individual to the development of glaucoma damage or the product of tissue remodeling induced by glaucoma damage cannot be determined in cross-sectional study of human eyes. To understand the effect of these material variations on the development of glaucoma, we are developing mouse models to study the relationship between the collagen/elastin structure and the mechanical properties of the sclera and their associations with glaucomatous optic neuropathy. Mouse models allows for in vivo manipulation of the intraocular pressure and longitudinal study of the effects of the baseline mechanical properties on the development of glaucoma axon damage and connective tissue remodeling. Furthermore, they provide important opportunities to manipulate the composition and structure of the ocular connective tissues by chemically treating the animals in vivo or by gene knockout techniques.
Our research aims to:
- Compare the effects of induced chronic IOP elevation on mechanical properties of the sclera and optic nerve damage.
- Perform experiments on multiple mouse strains to compare the effects of baseline properties on scleral remodeling and optic nerve damage.
- Compare effects of chemically and pharmacologically stiffening or softening the sclera on the development of glaucoma
- Develop micromechanism-based constitutive models for the growth and remodeling of the tissues in response to mechanical loading.

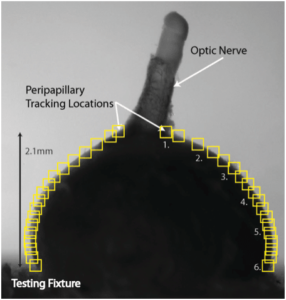
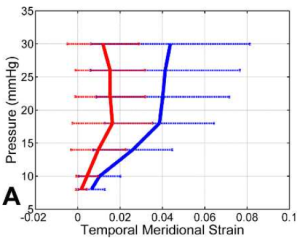
Figure 4: Inflation testing of the mouse eye, showing (a) the inflation test setup, (b) side view of the mouse eye marked for 2D DIC of the scleral edge, and (c) the applied pressure vs. meridional strain of the temporal edge comparing experimental glaucoma eyes (red) and the contralateral normal eye (blue). Glaucoma was induced by increasing the intraocular pressure in vivo for 6 weeks. This produced a significantly stiffer sclera.
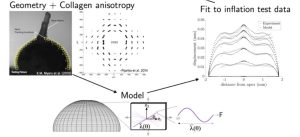
Figure 5. Schematic of the inverse finite element analysis used to fit the parameters of a micromechanical model of the sclera to the displacement field measured by 2D DIC in inflation tests.
Collaborators
- Craig Boote, PhD – Lecturer, School of Optometry and Vision Sciences, Cardiff University
- Harry A. Quigley, MD – A. Edward Maumenee Professor of Ophthalmology, Director, Glaucoma Center of Excellence, Johns Hopkins Medical School
- Ian Pitha, MD Assistant Professor of Ophthalmology, Johns Hopkins Medical School
- Brad L. Boyce, Ph.D. Sandia National Laboratories, Livermore, CA
- Reese Jones, Ph.D. Sandia National Laboratories, Livermore, CA

